Cognitive Behavioural Therapy (CBT) is actually quite difficult to define, as it can look very different when applied to different problems, for different individuals, by different therapists (or perhaps even computers, nowadays!). However, I think it is fair to say that the term refers to a family of talking therapies and approaches that are based on a common set of theories and principles. This can be hard explain in more general terms, so here I will try to apply it to some examples…
At its heart, CBT is based on the idea that emotional distress does not arise from events or experiences themselves, but rather the meaning we attribute to them. For example, a person suffering from depression may conclude they are a failure based on their interpretation of recent life events or childhood experiences, or someone suffering with social anxiety may believe that if people notice their anxiety they will be seen to be stupid, or weird. Whilst these beliefs will undoubtedly make sense based on the individuals own experiences, another person may believe that living through such life-events are signs of resilience or mean nothing about the individual, or that feeling nervous, blushing or stumbling on ones words is completely normal, meaning they are just the same as everyone else.
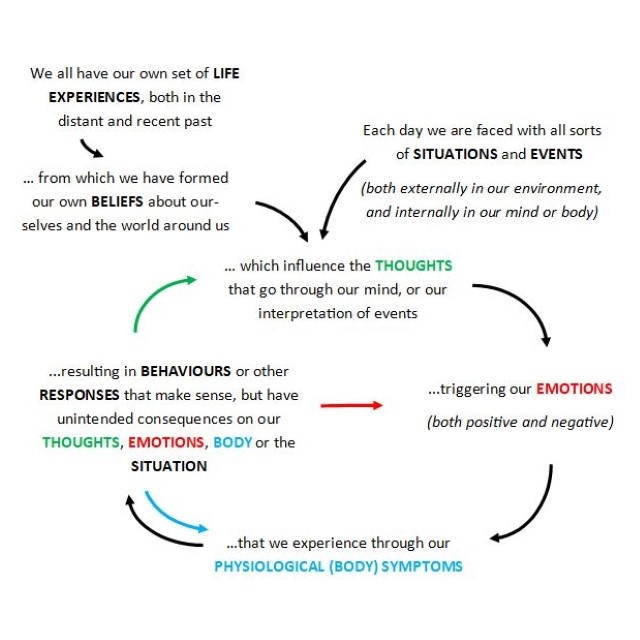
Cognitive Behavioural Therapists understand that we all hold our own set of beliefs about ourselves and the world, which influence the way we interpret and respond to our day-to-day experiences. These are constantly changing and evolving, based on the way we process information, for better or for worse! We can help you to draw on the scientific evidence for what maintains various mental health difficulties, both in terms of the beliefs you hold and the responses that could be maintaining them, so that you can make changes to break vicious cycles and free yourself from emotional distress. For example, the depressed individual above may have developed the rule to always put in 100% to ensure they are good enough, with the unintended consequences of feeling constantly stressed by overworking and the threat of failure, whilst never achieving the impossible 100% and reaching the same conclusion. The individual with social anxiety is likely to be so preoccupied with their thoughts and feelings and trying not to show their anxiety, that they are unable to fully engage in social interactions or process the information in their environment to learn that they are in fact acceptable to others.
In more practical terms, CBT therapy can look similar to other talking therapies, involving weekly sessions of approximately 60 mins, typically over 6-20 sessions. However, sessions may be more structured, including agreeing agenda items for each session, planning specific tasks to complete between sessions or taking notes on key learning. Importantly, a key aim is to collaborate as equal partners, to test out hypotheses and ideas to see what works best for each individual, as this will never quite look the same.
If you are interested to find out more then do keep a look out for future blog posts, where I will talk more about applying specialised CBT treatments for a variety of common problems, such as Social Anxiety, PTSD, OCD, Phobias, Insomnia and Depression. Otherwise, if you are ready to invest in your wellbeing, then book a FREE no-obligation 15-min consultation, or contact me via the website to discuss this further.